Coming to a dermatologist near you: The microscope will see you now.
We've heard a lot about liquid biopsies, but what if I told you non-invasive virtual ones are now a possibility?
Tissue biopsies are one of the most common diagnostic procedures.
If you’ve ever had a weird mole and gone to a dermatologist, they’ve probably cut a piece of it off (biopsy!) and sent it to a pathologist to figure out if it’s cancerous.
Biopsies are always invasive which is undesirable because they can be painful or leave scars even for benign things.
But what happens after the biopsy is taken is also pretty undesirable.
A pathologist doesn’t just put that chunk of your tissue under a microscope and shout, “Eureka, cancer!”
There’s a ton of preparation that happens before that!
The biopsy is embedded in paraffin, sectioned on a microtome (cuts insanely thin slices), stained with hematoxylin and eosin (H&E) and THEN it’s viewed by a pathologist.
This process can take days and it’s a highly skilled affair.
Wouldn’t it be easier if we could just peer into our skin directly with a microscope without all of the cutting, slicing and staining?
Of course it would, and that’s what the authors of today’s paper set out to do.
Microscopy techniques have advanced significantly over the past few decades and we can now see through multiple layers of skin.
These techniques include optical coherence tomography (OCT) or reflectance confocal microscopy (RCM), but interpreting images generated with these techniques requires training and they still have lower resolution than more traditional tissue section based microscopy.
To fix these problems, the authors used AI and machine learning to generate OCT images that looked exactly like their more labor intensive H&E counterparts.
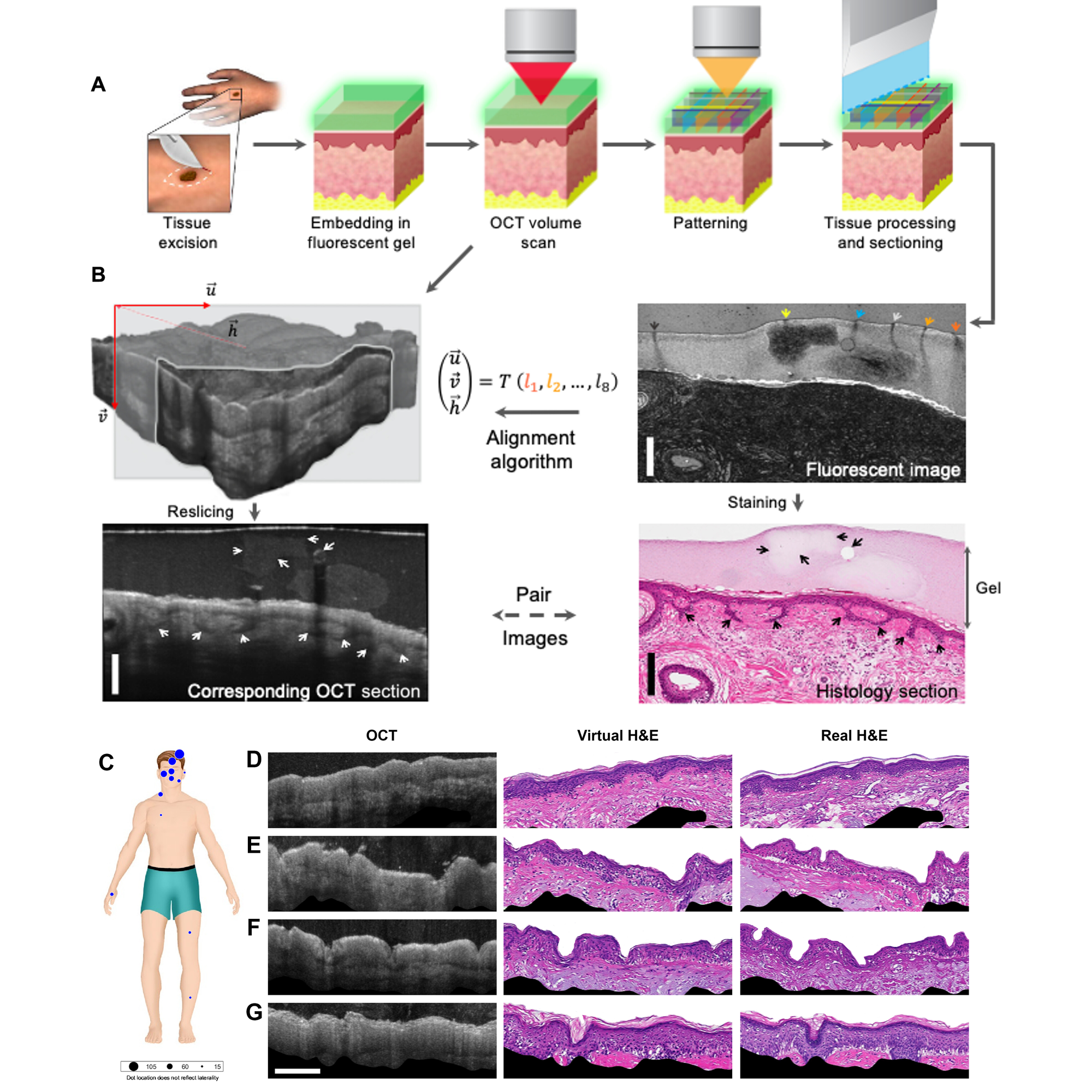
This work is detailed in the figure above.
In A) a traditional biopsy was taken, covered in a gel packed with fluorescent beads, scanned to make OCT sections and find the beads, and then the sample was sectioned and imaged normally.
This process generated the AI training data set seen in B) where OCT images with fluorescent bead markers were used to coregister (fancy word for lining up) them with the real H&E stained sections.
Finally, the trained algorithm was then used to generate virtual H&E stained sections (D-G) from OCT images of multiple skin biopsies (C).
While not perfect, the virtual biopsies were able to correctly ‘stain’ and identify complex structures like hair follicles with a resolution of 59 μm.
Further refinement of the technique with better training data and algorithmic optimizations are still required.
But a future that includes true virtual biopsies seems close, and could be key in enhancing our noninvasive diagnostic capabilities.
They'll also make trips to the dermatologist much more enjoyable!