Genomics is better with friends **cough** transcriptomics, proteomics, metabolomics, and epigenomics **cough**
Spoiler Alert: The future of disease early detection isn't going to be genomics
Spoiler Alert: The future of disease early detection isn't going to be genomics.
We already have some pretty good hints that this is true.
One of them is that many Multi-cancer early detection (MCED) screening tests are based on methylation.
This falls squarely in the realm of epigenomics.
But we also have three decades worth of high throughput genomics under our belts and we really don't have a ton to show for it.
We've certainly learned a lot in that time about the genome!
But one of the greatest lessons we've been taught is that genetics alone is terrible predictor of whether a healthy person will actually develop a disease.
Recent studies have shown that 8% of people carry a pathogenic mutation, but only about 7% of those people ever become symptomatic.
The caveat here being that some mutations are more likely to cause disease than others. These include mutations in BRCA1 and BRCA2 (Breast Cancer) or HBB (Thalassemia) in which 30-60% of patients with those develop disease.
So, what do we do with all of these 'damaging' pathogenic variants we find in healthy people?
The American College of Medical Genetics (ACMG) suggests extending the list of reportable findings to include pathogenic variants in 81 disease associated genes (inclusive of the 3 above).
These are all considered to be 'medically actionable' because steps can be taken to improve their clinical outcomes.
However, the struggle here, and with most genetic diseases, is knowing when, or if, a healthy person will ever become symptomatic.
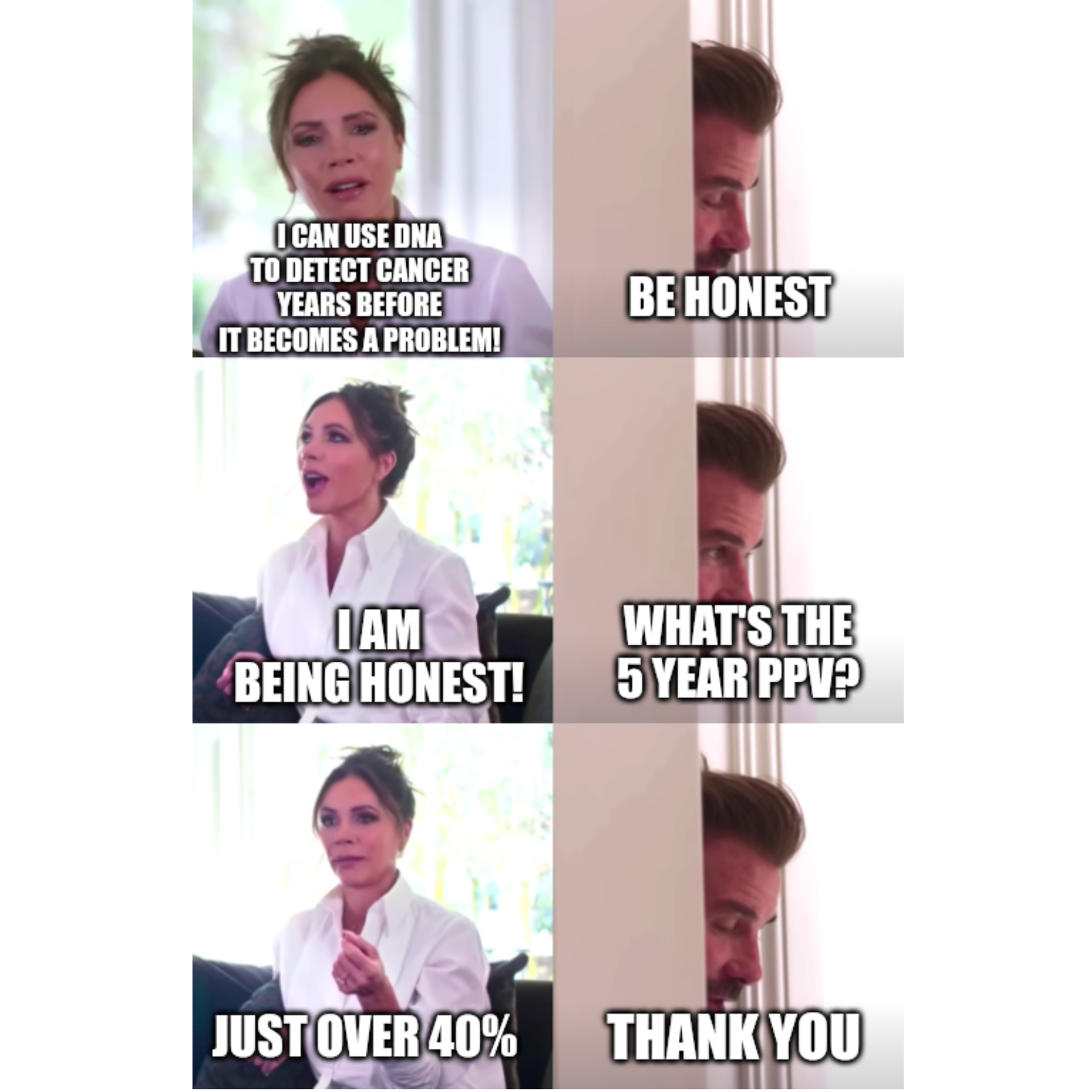
Wouldn't it be great if we had a way to detect disease onset decades before there's a phenotype in a patient?
We're finally at a point where this might be possible and it's all thanks to new developments in proteomics (the study of proteins and how they interact within our cells)!
Interest in proteomics has increased drastically in the past few years as new technologies have made it possible to easily study thousands of proteins in a single sample.
The power of these methods was highlighted in papers throughout 2023.
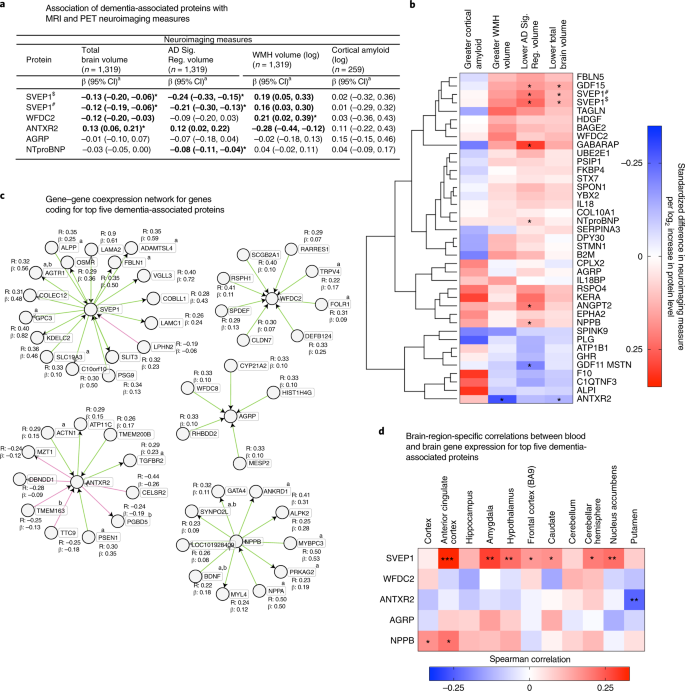
But one in particular stood out where the plasma of 11,000 patients who had participated in a 25-year study were screened for ~5,000 proteins.
The researchers were able to use samples collected during that original study to identify a set of proteins that could predict the development of dementia decades before symptom onset.
That's pretty incredible!
While there's still a lot of work to be done, it's exciting to see how proteomics continues to increase our understanding of the biology of disease.
Because, as we've learned, the genome only represents potential, but the proteome could tell us when, or if, that potential is actually beginning to impact biology!
