Expert panel on clinical microbiome use: "More evidence needed"
An international panel says clinical microbiomes aren't ready for primetime...yet
Microbiome testing has emerged in the last few years as one of the hottest new wellness trends.
And companies have sprung up that claim to be able to screen the microbes in your gut and provide recommendations for curing everything from food sensitivities to cancer.
I think most of us are aware that the majority of what these companies are promising is a fantasy.
And that's because the microbiome and our understanding of it are still in the earliest stages of development.
There's no question that the microbiome is important with respect to gut and immune health, metabolism, and our response to drugs, but just because we can test for something doesn't mean we understand it.
Nor is all of the data that is generated on this topic good data!
But that hasn't stopped companies from offering these services and providing guidance to consumers on how to use the results to hack their microbiomes.
Fortunately, there are those among us who approach the microbiome more seriously and understand that while we may not know much about the microbiome right now, there will likely be clinical diagnostic applications for it in the future.
What that means, though, is that the clinical community needs to come to a an agreement on how to perform and interpret microbiome testing in clinical practice.
That's why it was really interesting to see a consensus statement published a few weeks ago on the use of clinical microbiomes.
It was compiled by an expert panel of 69 microbiome researchers from 18 countries who see the potential of microbiome applications in the clinic but who worry about the current implementation of available tests.
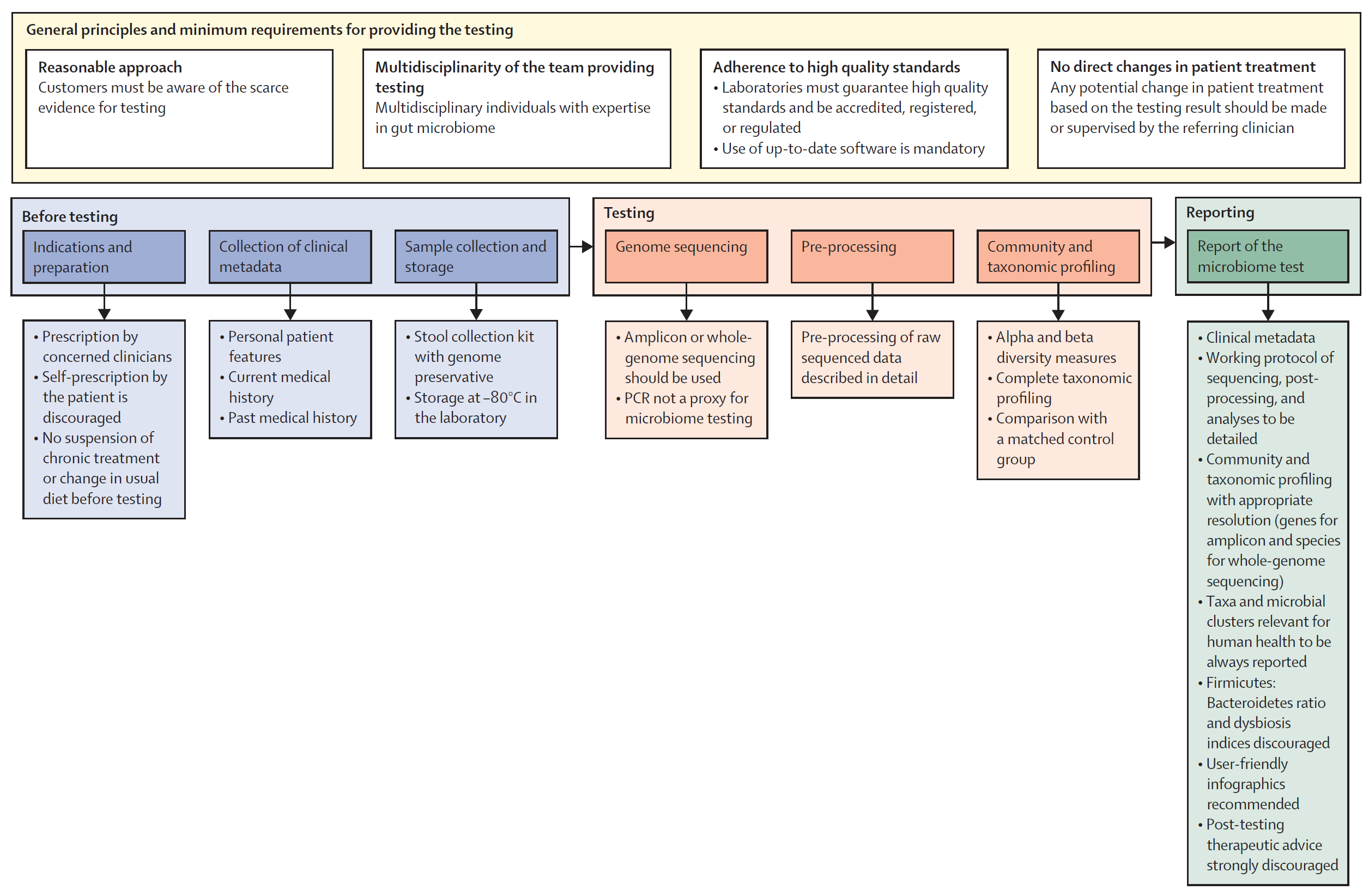
In the statement, they outline 5 key areas of importance (which I'll dig into) and provide a framework (Figure above) for implementing a microbiome testing program.
1. General principles and minimum requirements for providing diagnostic microbiome testing
The panel agrees that anyone prescribing a microbiome test should be upfront about the clinical and scientific validity of the test - specifically highlighting that there's limited evidence for the use of microbiome testing in the clinic. Since microbiomes are so complex, providers should have clinical teams with diverse backgrounds who understand the technology used and how to apply the results in clinical practice. The labs performing the testing should be of high quality, be accredited, regulated, use up-to-date bioinformatic pipelines, protect patient data and use non-proprietary laboratory and analysis methods that can be externally validated (🤔).
2. Procedural steps before testing
Since there is little clinical evidence for the use of microbiome testing, the intended use of the test must be clear and testing should only be performed under clinical guidance (no patient requests!). Essential clinical information such as "age, gender, BMI, dietary habits, smoking and alcohol status, gut transit time, comorbidities and medications, and past medical history" should be collected prior to testing to inform a proper diagnosis. Samples should be collected in a way that avoids contamination, they must be stabilized with a preservative, and stored appropriately at the lab (-80 C) prior to testing.
3. Microbiome analysis
Microbiome testing must be done by either amplicon sequencing (16S) or whole genome sequencing. PCR and culture based methods are not appropriate for getting a complete picture of a microbiome. Analysis pipelines must be well documented and report alpha and beta diversity along with community composition (as a percent). The analysis should also include a comparison to matched controls and, in specific clinical scenarios, longitudinal (sampling over time) may be appropriate to inform a diagnosis.
4. Characteristics of reports
The panel suggests that reports look like standard reports including a brief overview of the test method. Microbiome specific things to include are: alpha and beta diversity, community composition down to the deepest taxonomic resolution (phylum, genus, species, strain, etc...), and taxanomic shifts observed over time or compared to healthy matched controls. The panel discourages the reporting of a dysbiosis index, Firmicutes-to-Bacteroidetes ratio, "healthy" reference ranges, or any therapeutic advice (this should only come from a physician).
5. Relevance of microbiome testing in clinical practice: present and future
If it wasn't immediately obvious, this expert panel does not see much use for microbiome testing in the clinic except for in a few key scenarios (although, even in those ie H. pylori infection, they don't believe microbiome testing is strictly required...), but they do not discount the future potential of such testing and suggest that ongoing research on the microbiome's association with diseases is important. In the meantime, the panel suggests training clinicians on the basics of microbiome science and report interpretation to prepare for a future when the clinical evidence supports broader use of this type of testing.
