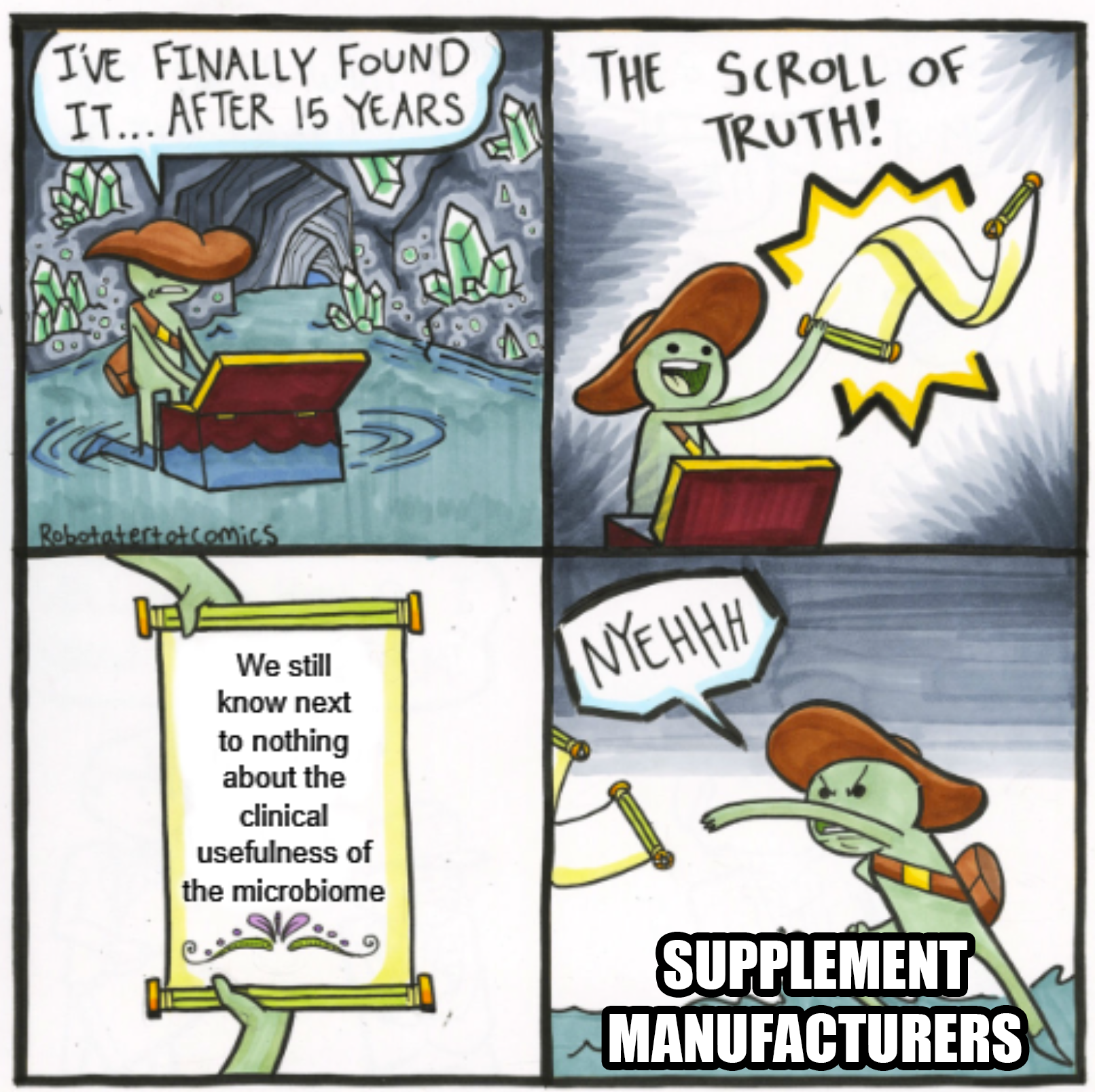
Clinical applications of the microbiome are still very much a work in progress
What's the clinical usefulness of a microbiome? We’re still trying to figure that part out!
The microbiome is composed of all of the fungi, viruses and bacteria that live on or in an organism inclusive of their omic interactions with one another.
Most discussions around the microbiome are related to health, wellness and disease, but to actually know anything about the clinical impact of the microbiome on those things, we need to do a lot of research!
There is broad agreement that the microbiome is important, but we currently have very little knowledge about ‘cause and effect’ or how broadly we can impact the microbiome to actually influence health or prevent disease.
And understanding cause and effect is very important because that tells us whether what we’re looking at when we sample a microbiome is just the ‘result’ or if it’s something we can manipulate to do our bidding.
Current research suggests it’s a little of both!
Inflammation - A dysregulated microbiome has been associated with skin rashes and mild to severe digestive problems. Much of this appears to be linked to metabolite production, some of which can activate the immune system to create undesirable side effects in the host, but create a more desirable living environment for the microbes.
Host Metabolism - Much of human microbiome research is focused on the gut microbiome and how the gut microbiome affects our ability to properly metabolize the food that we eat. We rely on bacteria to provide certain digestive enzymes and to help produce essential things like amino acids and vitamins that are not found abundantly in our diets.
Oncology - More recently, the microbiome has been studied in the context of oncology and how the tumor microenvironment might be influenced by bacteria - both in tumorigenesis and proliferation. But there is also ongoing research in how the microbiome might influence the effectiveness of cancer treatments because of how certain microbes metabolize chemotherapy drugs or modulate the immune system to reduce the effectiveness of therapies.
Pathogenic Infections - This is probably the space where we have the best clinical evidence. We know that pathogenic bacteria can cause major problems both on our skin (think MRSA) and in our digestive tract (think H. pylori or pathogenic E. coli). When these bacteria get a foothold, they take over but there is evidence that a healthy microbiome (or fecal transfer of one for gut infections) can resist these ne'er do wells.
While the sample sizes in most of these studies is very small, we’re just at the beginning of attempting to fully understand the role of the microbiome in health and disease.
Good data and properly designed studies are the first step in allowing us to make the important clinical associations that help us identify and/or engineer bacteria to fight disease or improve our health.
